Lactoferrin - a natural alternative for hay fever and allergic asthma?
Hay fever and allergic asthma
Duration: 3 minutes

Lactoferrin - a natural alternative for hay fever and allergic asthma?
Worldwide, about 25 % of the population is affected by pollen allergy or hay fever.[1] In Germany, about 12 million people (14.8 %) suffer from hay fever, which is the number one allergic disease. It usually affects the upper respiratory tract. The most common complaints include sneezing attacks, runny nose and itchy eyes, but also a decrease in performance, poor sleep quality and general exhaustion are among the accompanying symptoms.[2]
The allergic reaction is triggered by pollen or pollen from wind-pollinated plants. The main allergenic pollen comes from trees, grasses and herbs.[2]
However, after years of disease, a so-called "floor change" from the upper to the lower airways can also occur, in that the bronchi also react hypersensitively with the development of bronchial asthma.[2] The prevalence of allergic pneumonia has increased significantly in recent years, which is related to changing environmental factors such as inhaled pollutants (tobacco smoke, particulate matter, nitrogen oxides and ozone) as well as repeated exposure to respiratory viruses that produce reactive oxygen species (ROS).[1]
Oxidative stress is not only a consequence of environmental influences, but also arises during inflammatory processes, as inflammatory cells in the respiratory tract as well as in the blood vessels produce ROS. Physiologically, there is a balance between the production of ROS and its elimination that depends on the availability of transition metals such as iron. If there is an imbalance in this system due to excessive production of ROS, the cells become oxidatively stressed, which in turn leads to additional ROS production, changes in cellular signalling and the development of pathological processes. Iron can have a negative impact on physiological processes under conditions of oxidative stress, as its catalysing action converts superoxide anions (O2-) and hydrogen peroxide (H2O2) into cytotoxic hydroxy radicals. Pro-oxidative iron plays a role in oxidative stress in the lung in humans and animals.[1]
Lactoferrin (Lf) is known for its immunomodulatory and anti-inflammatory properties, as well as its action as an antioxidant. It is possible that Lf, due to its iron-binding capacity, can reduce the concentration of highly reactive species and thus reduce pollen-induced airway inflammation.[1]
In a cell culture study, Lf was shown to significantly reduce pollen-induced oxidative stress in bronchial epithelial cells.[1]
A subsequent in vivo study also showed therapeutic efficacy of Lf in mice with allergic airway inflammation [1]:
- The accumulation of eosinophils, immune cells belonging to the granulocytes and involved in cellular immune defence, was significantly reduced in the airways by Lf.
- The production of mucins (mucous substances) was reduced by Lf by decreasing the accumulation of mucin-producing cells.
- Airway inflammation was reduced by Lf decreasing the accumulation of inflammatory cells and mediators.
- The antioxidant effect already shown in cell culture was also confirmed in the mouse model by binding intracellular iron.
Another study showed in sheep with allergic asthma that inhalation of Lf can reduce both bronchoconstriction in the late phase and airway hyperreactivity. This is thought to be due to the physiological function of Lf to inhibit the release of tryptase, a messenger from activated mast cells (inflammatory cells). Tryptase is considered a possible cause of allergic asthma and the data from the study suggest that the messenger is involved in both bronchial constriction and airway hyperreactivity. Lf has been shown to bind to heparin, which is a stabiliser component of the tryptase molecule, and can thus exert its inhibitory effect.[3]
In addition to inhibiting the release of mast cell tryptase, it has also been investigated whether Lf can directly influence mast cell activation, a key factor in allergic reactions. Study results showed that Lf can inhibit immunoglobulin E-dependent histamine release from human mast cells by 50%.[4]
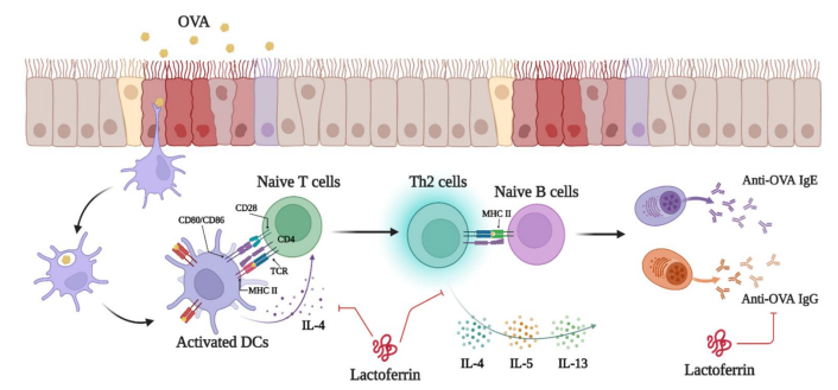
In the mouse model, further positive anti-inflammatory and immunoregulatory mechanisms of action of Lf in allergic asthma could be shown. The sensitisation of the mice and thus the triggering of the clinical picture occurred through ovalbumin (OVA).[5]
- Protective effect of Lf in ameliorating airway hyperreactivity and lung injury and inflammation.
- Reduction in the expression of Th2 cytokines (signalling molecules of the immune system; IL-4, IL-5, IL-13), the secretion of allergen-specific antibodies and the overall Th2 immune response.
- Influencing the function of dendritic cells (responsible for antigen-specific immune responses).
These results from initial in vivo studies with animal models provide promising evidence for a therapeutic benefit of Lf in allergic inflammatory diseases such as hay fever and allergic asthma. Clinical human studies are eagerly awaited.